Editor’s note: This is part of a periodic series of Health Affairs Blog posts discussing the Culture of Health, the topic of a November Health Affairs theme issue. In 2014 the Robert Wood Johnson Foundation announced its Culture of Health initiative, which promotes health, well-being, and equity. The initiative identifies roles for individuals, communities, commercial entities, health care entities, and public policy that extend beyond the reach of medical care into sectors not traditionally associated with health.
Policymakers, health plans, and provider organizations are aggressively pursuing care delivery and payment reforms in an effort to reduce burgeoning health care cost growth and improve health outcomes. Accountable care organizations (ACOs), coupled with capitated payment arrangements, have been billed as the next great hope.
As currently structured, however, most ACOs contain a serious flaw: Although there is now significant evidence of the value of investment in certain social services interventions, the vast majority of ACO financing structures, including most of those promoted by the Centers for Medicare and Medicaid Services (CMS) and state Medicaid programs, carve out the largest drivers of health: social, environmental, and community factors. Predominantly, ACO models focus entirely on traditional health care services, even though these services only contribute to a small proportion of an individual’s health.
At Commonwealth Care Alliance (CCA), the nation’s first “Social ACO,” we believe this is a mistake in terms of both health outcomes and cost containment. In our view, creating a “culture of health” through increased investment in social supports—combined with promotion of strong partnerships between traditional health care delivery and social services organizations in the form of fully financially integrated delivery systems—is the most important health care reform opportunity facing policymakers.
In contrast with most public-payer ACOs, which have emerged only recently and generally do not have integrated social services, CCA was an early pioneer in developing fully integrated models that address physical and behavioral health in tandem with social needs. More than a decade ago, CCA developed a delivery and financing approach that is rooted in community-oriented principles and that integrates medical and behavioral health spending with social services in the form of long-term services and supports (LTSS). The principles underpinning this model include the embrace of independent living as a primary goal; an affirmation of the dignity of risk; and the recognition that person-centered, community-based care for economically challenged populations with significant disease burdens must comprehensively address of all the challenges they face, not just those rooted in the traditional medical model.
Today, CCA cares for almost 19,000 individuals who are dually eligible for Medicare and Medicaid. Our patients have substantial disabilities, and many are frail elders. They are poor and often disenfranchised. Some are homeless, and many are homebound. Nearly 80 percent of our members have a behavioral health disorder alongside their complex physical illness.
Yet for all their medical issues, our patients’ social and economic challenges frequently outstrip their medical needs by far. Consistent with the findings of Taressa Fraze, Elliott Fisher, and colleagues in their November Health Affairs paper exploring the social services provided by Medicare and Medicaid ACOs, transportation, food security/malnutrition, and unemployment are the concerns that most directly affect our patients’ health and our spending; social isolation, loneliness, and lack of community engagement also play a significant role in driving health-related behaviors and clinical outcomes.
Reflecting these realities, the fully integrated, person-centered view of a true Social ACO, including direct investment in population-wide interventions that can be adapted to meet the needs of each individual consumer, produces tangible clinical and financial benefits. When we look across the landscape of ACOs in both Massachusetts and beyond, however, we see little cause for optimism that these trends are taking hold. Instead, integration of social factors in most delivery systems is an afterthought — comprising, at best, a patchwork quilt of connections to disparate social agencies that may or may not be optimally positioned to meet an individual patient or family’s needs.
What Do Most ACOs Attempting to Integrate Social Services Look Like Today?
As reported by Fraze, Fisher, and colleagues, in most publicly financed (Medicare and Medicaid) ACOs, “approaches to meeting patients’ non-medical needs were either individualized solutions…or targeted approaches;” moreover, “only people who were engaged with the medical system had the opportunity to be involved in an ACO’s non-medical programs.” In Massachusetts, while our state Health and Human Services administration has admirably sought to encourage the comprehensive integration of social factors into their new Delivery System Reform Incentive Program (DSRIP) and Medicaid ACOs, the traditional delivery system has resisted.
Among the explicit stated goals of the MassHealth DSRIP proposal is “improved integration among physical health, behavioral health, long-term services and supports, and health-related social services.” Yet Massachusetts’ largest delivery systems and health plans have expressed skepticism and resistance to the idea that small community-based providers may be optimally positioned to drive care for a given individual.
A second issue is control: Traditional delivery systems commonly assert that they must bear ultimate responsibility for all decision making related to those patients for whom they’re at risk financially. Thus, the resulting partnership model is often more of the same: traditional delivery and payment systems bear increased financial risk for medical delivery of care and “refer out” any socially related needs of their patients, without an associated transfer of decision making or financial risk to their downstream, community-based partners.
A critical barrier in this regard, beyond the cultural blinders that may be found in the traditional medical model, is that most ACOs currently do not provide for or require full integration of social financing through such funding streams as states’ LTSS programs. Here, Massachusetts state officials have persevered — stipulating that by 2020, LTSS, medical, and behavioral health spending must be fully integrated in Medicaid ACO models, with providers bearing financial risk across the continuum.
Finally, despite early efforts in structure and financing, the current prevailing environment demonstrates the continuing absence of a cultural and structural conversion to a view that social facets of care are as important as traditional health care services. This lack of appreciation for the immense role of social determinants of health may prove to be the critical obstacle to the expansion and sustainability of fully integrated care and, ultimately, to the realization of improved health outcomes for society’s most vulnerable members.
What Should Most Social ACOs Look Like? Our Vision
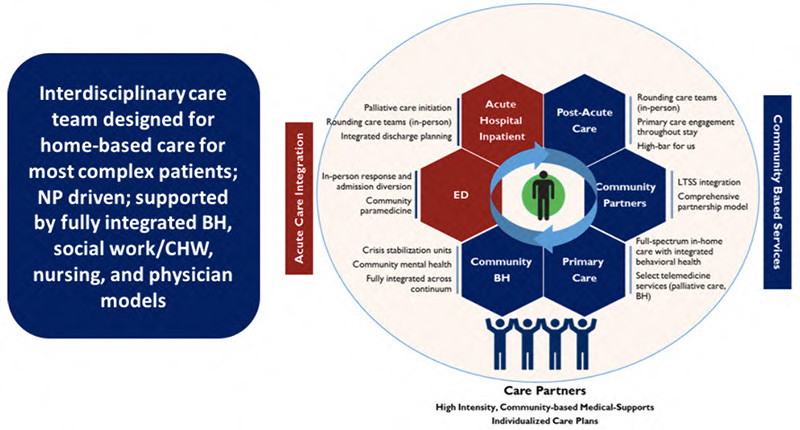
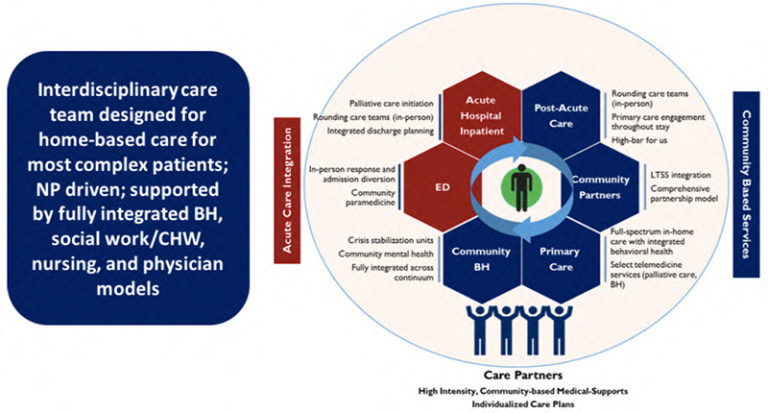
As a fully integrated health plan and delivery system, CCA has had the unique opportunity to develop a revolutionary care model, with resulting lessons for stakeholders across the nation. Our model of person-centered, community-based care for our most complex patients is grounded in the concepts of comprehensive care coordination and enhanced primary care.
Moreover, as a health plan, we fully integrate premium dollars into our medical, behavioral health, and social (LTSS) spending. We can just as easily use “medical dollars” to pay for our members’ air conditioners in order to prevent asthma, or for medically tailored meals that support patients with diabetes, as for inhalers and insulin to treat their downstream symptoms. This allows us, working within our organization and under the control of individual primary care providers and care managers, to rebalance the ratio of spending on social supports versus medical care that, as reported by Elizabeth Bradley and colleagues, differentiates the United States from our western European counterparts.
The core components of CCA’s care and financing model demonstrate opportunities for emerging social ACOs and for policymakers.
Trusting, longitudinal relationships
CCA’s care model is based upon engaging each member to identify their comprehensive human needs, including medical, behavioral health, and social, and making the connection between disease states, the traditional delivery system, and each person’s ecosystem. Each CCA member is assigned a Care Partner — a member of CCA’s care team who builds longitudinal, trusting relationships with members.
Within the first weeks of enrollment, member needs related to social supports are documented directly in each member’s comprehensive care plan alongside medical and behavioral health information. The Care Partner then leverages a comprehensive team of clinical and non-clinical staff, as well as community partners—in particular, CCA relies heavily on community peers and health outreach workers—to walk hand-in-hand with the member as he or she accesses various care systems. This human integration is integral to providing members with care that is tailored to their needs in consistent, systematic ways.
Fully integrated financing of medical, behavioral health, and social supports through global capitation
Full financial integration is the single most powerful aspect of social ACOs, and one that must be adopted nationally. In particular, the ability to directly balance community-based investments with acute care savings allows greater investment in primary care and social services. In the zero sum game that health care traditionally represents, this forced redistribution through capitation is likely to be the primary mechanism through which we can rebalance spending on medical versus social factors.
A longer time horizon for measuring impact
We must recognize, as many have previously demonstrated, that the time to measurable clinical and financial impact from social investments such as the treatment of homelessness or social isolation is fundamentally different from, and longer than, the time to measurable impact of, say, an appendectomy. This idea is easy to understand conceptually but exceptionally challenging to implement. Social ACOs will need to (and need to be allowed to) pursue alternative retention incentives that enable them to increase their likelihood of realizing returns on non-medical investments.
Initial studies of the investment arc throughout the first three years of a member’s engagement with CCA demonstrate that, in populations with complex needs in particular, early investment is critical to meet pent-up demand and that on average this investment does not yield savings until 18-24 months of enrollment with our health plan. Thus, high-volume churn is destructive to our social service investment model. Moreover, lack of investment in these supports (as measured through members that refuse engagement with our health plan) leads over time to disproportionately higher spending, most likely through uncontrolled catastrophic events and progressively worsening chronic illness.
Fierce commitment to community-based delivery of social services with bi-directional integration
At CCA, we emphasize tight linkages with social services entities as opposed to building replacement services ourselves. Staff representatives of community partners are embedded directly within our care teams at CCA’s expense (see Exhibit 1). We rely heavily on geriatric support services coordinators and other LTSS staff from organizations such as area agencies on aging and independent living centers. This commitment builds trust and empowerment. We have also developed financial incentives that enable alignment with those community partners while protecting them from levels of financial risk that they cannot bear as small organizations. This innovative model has had a profound impact: We have high member satisfaction and lower acute care utilization than comparable populations in traditional Medicaid or Medicare managed care.
As reported in Health Affairs Blog by our colleagues, Melinda Abrams and Donald Moulds, however, allowing traditional health care organizations to address their patients/members social needs in isolation carries significant risk. When it comes to investment by the traditional delivery system in social services, we must maintain an approach that empowers community-based providers through financial support, shared governance, and bi-directional information sharing. Tools such as health information exchanges can also empower community-based organizations, but only if investments are made to make these tools truly bi-directional. Only by deconstructing the power differential between the traditional delivery system and community-based services can we achieve true integration. In the final analysis, the financial value of enabling social services providers in these ways is likely to be profound; after all, the health care sector is notoriously inefficient, and the easiest way to add costs is to medicalize services.
Innovating and breaking down siloes
At its core, trite though it may sound, person-centered care requires person-centered approaches. As health systems begin to incorporate social services and financing into their traditional structures, new staff capabilities must be developed that enable and empower case workers and community-based providers to make flexible decisions in support of community-based care.
Semi-structured aspects of financing—for example, paying $25 for a babysitter so that a mother can get effective education on how to manage her child’s asthma—may yield unprecedented dividends. Approaches such as the one being piloted by the Massachusetts Health Policy Commission’s CHART program, which allows community hospital-based case workers flexibility to spend modest sums for transportation, child care, or even rent—all without authorization-like processes—are powerful. Organizations with financial alignment also will stop at nothing to achieve the potential value available to them. We must harness that organizational drive to increase access to high-quality social supports.
Considerations for Policymakers
As health care leaders across the nation grapple with reform efforts, Social ACOs must be at the forefront of the discussion. In our own state of Massachusetts, we see traditional delivery systems and health plans grappling with how to achieve deeper integration of social supports into health care. We are optimistic that over time, reforms will increasingly prioritize two essential components: capitated payment models that incorporate social spending, and care delivery models that address unmet social needs alongside medical care needs. Achieving this will require alternative policies and contracting models from state agencies that oversee social supports, as well as close partnerships between delivery systems and social services agencies.
We must weave whole-person health throughout the accountable care framework. Only then will we achieve true care integration that improves health outcomes while reducing the total costs of care.
Exhibit 1