Doctors of osteopathic medicine have been around since the late-1800s but are gaining increasing attention due to their recent dramatic growth. While doctor of osteopathic medicine training was originally more focused on spinal manipulation, today it is very similar to the training for medical doctors and accepted as equivalent by state licensing agencies and most residency programs. The Accreditation Council for Graduate Medical Education (ACGME) and the American Osteopathic Association (AOA) have teamed up to establish a single accreditation system for all graduate medical education (residency) programs. By 2020, the single accreditation system will further narrow the distinction between medical doctors and doctors of osteopathic medicine as all residents and fellows will have to meet the same training standards.
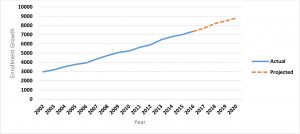
Doctors of osteopathic medicine currently make up about 8.5 percent (N = 81,115) of licensed physicians, but that percentage will increase in the coming years. After doubling osteopathic medical school enrollment over the past decade, doctors of osteopathic medicine now comprise 26 percent of first-year medical students in the United States with further increases expected, as shown in Exhibit 1 below. As a consequence of this growth, doctors of osteopathic medicine represented approximately 17.6 percent of physicians entering the graduate medical education pipeline in the United States in 2015 when factoring in doctors of osteopathic medicine beginning residency training in ACGME-accredited residencies (N = 3,347) and the approximately 2,000 that entered AOA-accredited residencies (Note 1).
Despite concerns among some academic medical leaders that the increase in medical school graduates will lead to more students not being matched in ACGME residency training programs, the match rate for doctors of osteopathic medicine in the National Resident Matching Program (NRMP) grew from 75 percent to 82 percent between 2013 and 2017 even though the number of doctor of osteopathic medicine applicants increased by 24 percent (2,677 to 3,590). In 2017, 99 percent of graduating doctors of osteopathic medicine seeking graduate medical education were matched, with approximately 52 percent entering through the NRMP, 43 percent through the AOA match, and the balance through the military match and other match placements, such as the SF (San Francisco) Match.
Exhibit 1: Osteopathic Medical School First-Year Enrollment Growth, 2002–20

Sources: Schulman SA, Levitan T, Dill MJ. Key indicator in academic medicine: matriculants to medical schools in the United States. Acad Med. 2012;87(2):240–1; 2012, 2013, 2014, and 2015 Association of American Medical Colleges’ Medical School Enrollment Reports.
The Single Graduate Medical Education Accreditation System
The ACGME and the AOA are transitioning to a single accreditation system, which will be fully implemented in 2020. Accredited AOA programs are in the process of application and review by the ACGME. Currently, only doctor of osteopathic medicine graduates can apply for AOA residency training programs, but the single accreditation system will allow medical doctor graduates (including international medical graduates) to also apply for all residency slots. However, medical doctors will need to meet prerequisite requirements for programs with “Osteopathic Recognition.” This could make training programs, which were previously only accredited by the AOA, more competitive and impact future match rates for both training pathways. However, there is a concern that some rural AOA residency programs may close as a result of single accreditation, potentially reducing the number of trainees who are likely to practice in rural areas.
Background On Current Student Profile
Between 2009 and 2016, the percentage of females matriculating in an osteopathic medical school has decreased slightly from 47 percent to 46 percent, while the number of under-represented minorities increased from 7 percent (337) to 8.5 percent (577); an increase of 71 percent in terms of actual matriculants. Among the 2016 entering students, 21 percent are from a small town or isolated rural area, 13 percent are the first in their family to attend college, and 8 percent are from a family that received public assistance (for example, aid to families with dependent children, food stamps, Medicaid, public housing) or personally received public assistance. Average MCAT scores and GPAs have been rising slightly along with the increase in doctor of osteopathic medicine enrollment—an indication that admission standards remain high.
Distribution
Data show that medical school location has a major impact on ultimate practice location. The majority of doctor of osteopathic medicine schools are located in health professional shortage areas or medically underserved areas. A number of schools are in mid-size cities in rural areas, such as Tulsa, Oklahoma, and Fort Smith, Arkansas, and in smaller, rural communities, such as Dothan, Alabama; Kirksville, Missouri; and Lillington, North Carolina.
Such locations increase the likelihood that graduates will end up practicing in rural and underserved locations. While doctors of osteopathic medicine practice in all 50 states, 86 percent of doctors of osteopathic medicine are located in one of the 27 states with a doctor of osteopathic medicine school as of July 2015. In the past two years, the number of schools has continued to increase, and there are now doctor of osteopathic medicine schools in 31 states. State variation in the percentage of doctors of osteopathic medicine in the workforce ranges from a low of 1.4 percent in Louisiana to a high of 20.9 percent in Oklahoma, as shown in Exhibit 2 below.
Exhibit 2: Percentage Of Doctors of Osteopathic Medicine In The Physician Workforce, By State
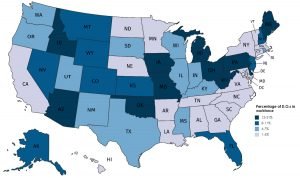
Source: Association of American Medical Colleges State Physician Workforce Data Book, 2015. Note: D.O. is doctor of osteopathic medicine.
Doctors Of Osteopathic Medicine And Primary Care
As the nation grapples with concerns over primary care shortages, it is important to note the role doctors of osteopathic medicine play in the primary care supply. Nearly half (45 percent) of doctors of osteopathic medicine practice primary care, and they account for 10 percent of all primary care physicians. In comparison, 34 percent of medical doctors are primary care physicians.
There is some concern about the declining percentage of doctors of osteopathic medicine practicing primary care, which is also a concern among medical doctors. In 2015–16, the majority of doctors of osteopathic medicine (59 percent) entered ACGME residency training in a family medicine, internal medicine, or pediatric residency program compared to 41 percent of US medical doctors and nearly three out of four (73 percent) international medical graduates. Some will go on to pursue subspecialty training, further reducing those numbers. Doctors of osteopathic medicine also have a second pathway for pursuing primary care through AOA-accredited residencies, which are not included above.
Nonetheless, a 2015 report by the American Academy of Family Physicians shows that the percentage of doctor of osteopathic medicine graduates in primary care has been declining from highs of 56 percent of doctor of osteopathic medicine graduates in the mid-1990s during the height of managed care to 42 percent in primary care among more recent graduates. Over the past few years, student interest in primary care careers as been relatively low with only one in five doctor of osteopathic medicine matriculants stating an interest in a career in primary care. While more doctor of osteopathic medicine students graduate with intentions to practice primary care than did when entering medical school, the percentage of doctors of osteopathic medicine who ultimately become primary care physicians could potentially drop even lower in future years.
Conclusion
The doctor of osteopathic medicine workforce is growing rapidly with no signs of decreases in the quality of students accepted or their success in matching into a residency training program, which has been steadily rising. Given the doctor of osteopathic medicine workforce’s higher likelihood of practicing in rural communities and of pursuing careers in primary care, doctors of osteopathic medicine are on track to play an increasingly important role in ensuring access to care nationwide, including for our most vulnerable populations.
Note 1
Since some residencies are jointly accredited by both the ACGME and the AOA, it is difficult to determine the number of residents that are AOA-accredited only. Using 2015 data, the authors worked backwards to estimate the number of doctors of osteopathic medicine entering residency by estimating 98 percent of doctor of osteopathic medicine graduates (5,472 x 0.98) entered residency training, subtracting out the number known to enter ACGME (3,347) to thereby estimate the number entering AOA residency programs (2,016), and adding that to the number of ACGME residents entering the pipeline (28,456) to get the total number of residents entering the ACGME and the AOA pipeline (30,472).
Authors’ Note
Ms. Erikson previously received limited financial support from the American Association of Colleges of Osteopathic Medicine to review and compile data on the osteopathic workforce.