Breast cancer is a terrifying disease for most women. In the United States, it is the leading cause of cancer deaths among women ages twenty to fifty-nine years. More than 5,100 women are diagnosed with—and at least 1,100 women die from—breast cancer in New York City each year. The breast cancer survival rate is also lower for uninsured women than for those with private health insurance coverage.
Although access to affordable breast cancer screening and treatment has grown substantially over the past few years as a result of increased health insurance coverage options through the Affordable Care Act (ACA), many uninsured women are not able to obtain free or subsidized screening and treatment—in New York City and across the country as well—largely because of age and income-eligibility requirements that must be met to participate in cancer screening and treatment financial support programs.
In New York City, a partnership-based payment and delivery system model designed for breast cancer called the Breast Treatment Task Force (BTTF) has facilitated more than 6,000 screenings and diagnostic procedures and seventy-one cancer treatments for more than 3,500 patients over the past decade.
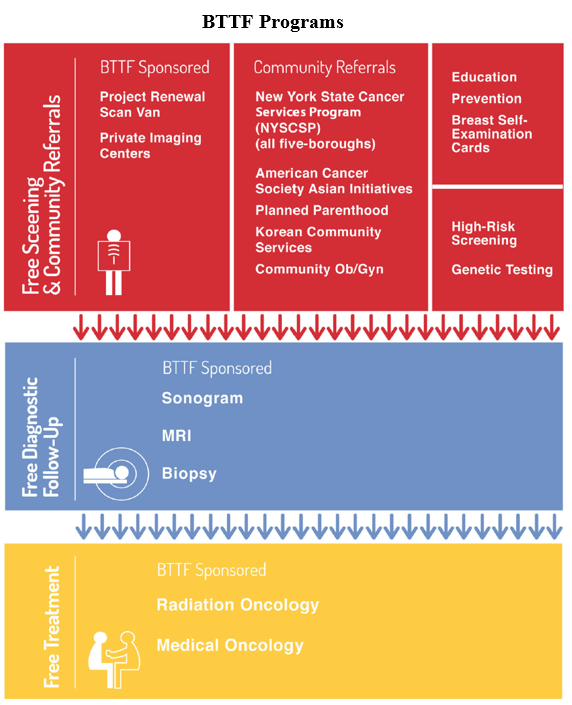
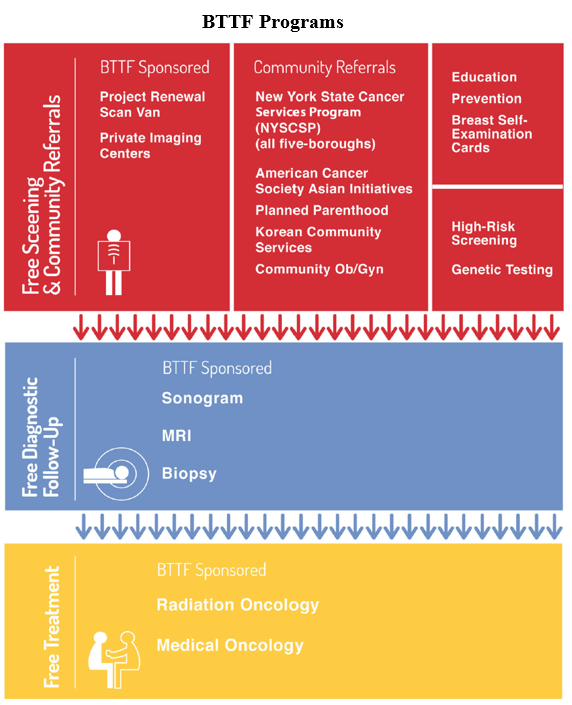
The BTTF is a nonprofit organization that facilitates breast cancer screening, education, diagnostic follow-up, and treatment for women without health insurance coverage. Most diagnostic and treatment services are provided to the BTTF free of charge by physicians, hospitals, imaging and radiology centers, and pharmaceutical companies, while other costs are covered through grants and donations from foundations (Avon Foundation for Women, Sy Syms Foundation, Harry S. Black and Allon Fuller Fund, and Investors Foundation) and other organizations (Barbells for Boobs and Pfizer).
Which Patients Fall Through The Cracks?
There is no question that high-quality cancer care depends on the ability of people to secure, travel to, and pay for needed diagnostics, treatment, and support services. While the Cancer Services Program of the New York State Department of Health provides cancer screening to uninsured and underinsured men and women throughout the state, many patients still fall through the cracks. In the case of breast cancer, that program provides mammograms and clinical breast exams at no cost to women ages forty and older, while younger women must wait for a health care provider licensed in New York to determine their eligibility for those services. This can mean anything from providing proof that one has multiple, close blood relatives who have been diagnosed with breast cancer in the past (like an aunt, mother, or sister), to demonstrating that one has a personal history of receiving thoracic (chest) irradiation as a teenager.
Other patients who often fall through the cracks are low-income women who are ineligible for Medicaid or other state or federal assistance programs. This population remains uninsured because health insurance premiums can be as high as $5,000 per year. Thus, even if they suspect they have cancer or are actually diagnosed with it, they have few options when it comes to receiving follow-up testing and treatment.

Lastly, while the ACA has ensured that people do not pay out-of-pocket costs for most cancer preventive services, most health insurance plans still do not fully cover some preventive services such as testing for the breast cancer (BRCA) gene. This is the case because most patients must be classified as high-risk first before undergoing such genetic testing, and, for most women, this means that they must have a prior diagnosis of cancer before age forty-five or have one or more close blood relatives who have been diagnosed with ovarian, pancreatic, prostate, or breast cancer. These restrictions increase the number of cancer patients who remain at risk, especially uninsured women who cannot afford to pay the out-of-pocket expense of BRCA testing, which ranges from $475 to $4,000.
How Does The BTTF Model Work?
The BTTF facilitates breast cancer screening, diagnostic follow-up, and treatment for women of all ages in New York City who are usually ineligible for the state-run Cancer Services Program. The BTTF assists with ultrasounds, biopsies, magnetic resonance imaging (MRIs), and other necessary diagnostic follow-up procedures for low-income, uninsured patients who cannot afford or access these services. In-kind donations to the BTTF by private imaging and radiology centers typically cover more than 75 percent of the costs of diagnostic follow-up. The BTTF also facilitates free surgeries and chemotherapy treatments for uninsured breast cancer patients. About 95 percent of the treatment costs are donated by surgeons, pharmaceutical companies, and hospitals.
Why Do Imaging and Radiology Centers And Other Health Care Providers Support The BTTF?
The BTTF coordinates the provision of services through private imaging and radiology centers and other health care providers (for example, Lenox Hill Radiology, CP Advanced Imaging, Bay Ridge Medical Imaging, Ralph Lauren Center for Cancer Care, Bellevue Hospital, and Woodhull Hospital, among others) in a way that minimizes disruption in the delivery of health care services to everyone else going to these providers. For example, the BTTF may coordinate the provision of patient services at a time in which a given private imaging or radiology center can best accommodate appointments. The BTTF also limits its requests for services to a volume that can be managed appropriately by imaging and radiology centers.
Is The Model Scalable And Replicable?
The short answer is “yes.” At least in New York City, imaging and radiology centers seem to be willing and able to handle more BTTF patients than they do already—with very limited disruption to their day-to-day operations and without affecting the services they provide to other patients. Although we believe that the BTTF model can be replicated successfully in other communities across the nation, successful adaptation and dissemination of the model requires careful attention to the development of sustainable partnerships with imaging and radiology centers and other health care providers. Growing the patient pipeline too fast in busy imaging and radiology centers may affect these facilities’ willingness to participate and, thus, affect sustainability of the model.
Lastly, the BTTF relies on partnerships with foundations and other donors.
Continuous cultivation of relationships with the types of partners we have mentioned and being acutely aware of the need to provide breast cancer screening, diagnostic, and treatment services that are aligned with the missions of the different organizations involved are critical elements to the success of the model.