The June issue of Health Affairs explores the topic of behavioral health, including racial and ethnic disparities in treatment, trends in financing of behavioral health and substance use disorder treatment, the portrayal of mental health issues in the media, and more.
This month’s DataGraphic provides a pictorial view on behavioral health becoming a focal point in policy and public discussions.
The June issue of Health Affairs is supported by the California Health Care Foundation; Takeda Pharmaceutical Company, Ltd.; the Leona M. and Harry B. Helmsley Charitable Trust; and the Conrad N. Hilton Foundation.
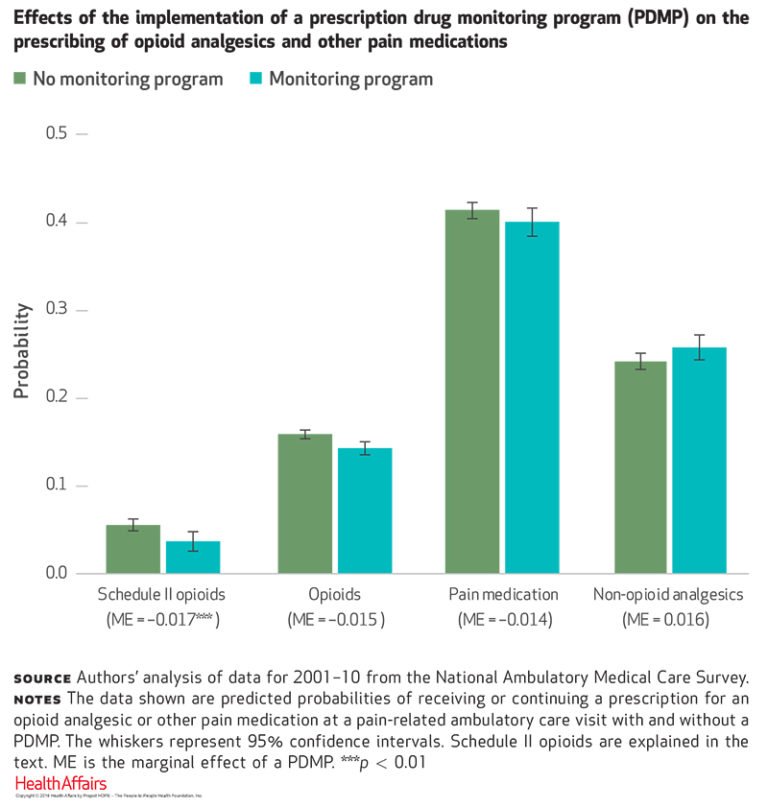
Drug monitoring programs associated with sizable decrease in Schedule II opioid prescriptions
Implementation of prescription drug monitoring databases by states is associated with a reduction in the likelihood of physicians prescribing a Schedule II opioid at an office visit for pain. Using data from the National Ambulatory Medical Care Survey covering the experience of 24 states over 10 years, Yuhua Bao of Weill Cornell Medicine and coauthors found that the launch of such monitoring programs was associated with a 30.0 percent reduction in the rate of prescribing Schedule II opioids.
The authors suggest that launching the programs may have substantially raised awareness among prescribers about controlled substance misuse, leading to more cautious prescribing patterns among prescribers who did not use the programs. While the authors say that further research is needed to monitor recent trends, they conclude that these drug monitoring programs show promise in reining in the epidemic of prescription opioid overdose.

DATAWATCH: Treatment for mental health is increasing, but disparities remain
Mental health treatment rates increased significantly in 2014 among those experiencing serious psychological distress, but racial and ethnic disparities in access to mental health services persisted. Timothy Creedon of Brandeis University and Benjamin Lê Cook of Harvard Medical School examined data from the National Survey on Drug Use and Health to evaluate access to behavioral health treatment associated with early implementation of the Affordable Care Act’s Medicaid expansion and state health insurance exchanges.
While respondents were significantly more likely to receive mental health treatment than those in earlier comparison periods (2005–13), racial/ethnic minority respondents continued to receive treatment at substantially lower rates than whites. The authors suggest that gains in insurance coverage alone are unlikely to push forward meaningful reductions in mental health treatment disparities.
A related study in the June issue:
Mental health treatment shifts to insurance financing, contrasts substance use disorder treatment
Spending data on mental health services reveal a long-term trend of increased financing of mental health care by insurers (private, Medicare, and Medicaid)—from 44.0 percent of total mental health spending in 1986 to 68.0 percent in 2014. In contrast, the majority of substance use disorder treatment was funded through state and local government budgets and out of pocket by consumers.
The study, conducted by Tami Mark of Truven Health Analytics and coauthors, also revealed that from 2004 to 2013, a growing percentage of adults received mental health treatment, albeit only because of the increased use of psychiatric medications. In the same period, only 1.2–1.3 percent of adults received substance use disorder treatment in any setting, although use of medications to treat substance-related disorders increased rapidly.
Gun violence and mental health—a missed opportunity for prevention?
Looking at laws that prohibit gun possession, researchers found that 20.9 percent of a study population with serious mental illnesses lost their gun rights as a result of a felony criminal record, while 12.8 percent were disqualified because of a mental health legal record.
Jeffrey Swanson of Duke University School of Medicine and coauthors studied 81,704 adults diagnosed with schizophrenia, bipolar disorder, or major depressive disorder in two large Florida public behavioral health systems from 2002 to 2011. They found that 62.0 percent of violent gun crime arrests and 28.0 percent of gun suicides involved individuals who were illegally in possession of a gun at the time. The authors conclude that comprehensive solutions will be required to meaningfully reduce the problem of gun violence and suicide, including enacting risk-based gun removal laws and prohibiting people who had been involuntarily detained in short-term psychiatric hospitalizations from owning guns.
News media disproportionately associate violence with mental illness
Amidst growing national awareness of mental health in the US, researchers warn that the news media’s disproportionate coverage of interpersonal violence associated with mental illness can be misleading. Using a random sample of 400 US news stories about mental illness from 1995 to 2014, Emma McGinty of the Johns Hopkins Bloomberg School of Public Health and coauthors found that more than one-third of all news stories about mental illness—38.0 percent—linked mental illness with interpersonal violence.
While the prevalence of stories on interpersonal violence did not change over the period studied, the stories were more likely to appear on the front page of a newspaper in the second decade of the study period, emphasizing the rate of violence in a way that the authors state is highly disproportionate to actual rates among the US population with mental illness. They recommend an increase in news media depictions of successful treatment for and recovery from mental illness — which made up only 14.0 percent of news stories.